What is Microsurgery
Sometimes, your body needs "reconstruction." This can happen when your body does not form in a standard way, when you have an injury (like a trauma), or when you have surgery that removes important tissue. When you are missing tissue that is important either for your body's functioning or appearance, your plastic surgeon might mention "microsurgery."
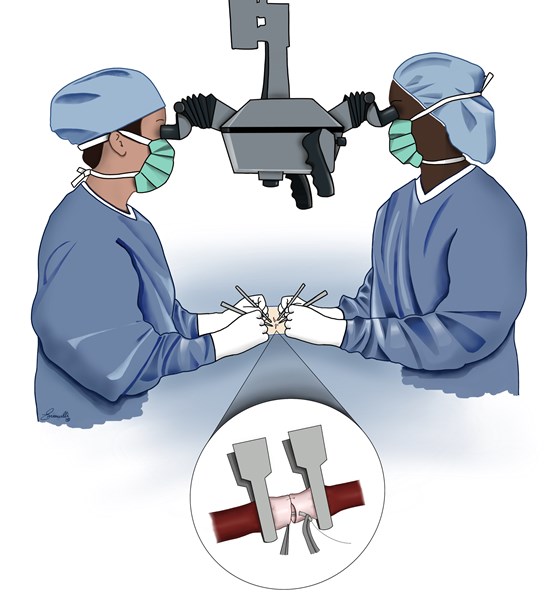
"Microsurgery" is a type of surgery that allows your own tissue to move from one place on your body to another place on your body. This can be useful if the area of your body that needs reconstruction does not have extra tissue nearby. The surgery itself needs "donor" tissue that can be moved to the "recipient" site (the part of the body that needs reconstruction). When the "donor" tissue is far away from the "recipient," surgeons often need to use a microscope to operate on blood vessels to keep the surgery successful. Using a microscope (or other magnifying lens) for surgery (usually to connect blood vessels) is called "microsurgery."
What are "flaps & free flaps"?
When you need reconstruction surgery with a plastic surgeon, this might mean that tissue is missing from a particular place on your body. A piece of tissue that is being used in surgery to replace what is missing is called a "flap." "Flap" tissue that is being moved from one place to another in surgery must have a good blood supply before, during, and after the surgery. Your plastic surgeon will recommend a surgery designed to keep the "flap" blood supply strong. Sometimes, the tissue on your body needed for your "flap" is far away from the part of your body that is being reconstructed. When this happens, the "flap" may be entirely disconnected from your body for a short time during your surgery and then reconnected to your body. This type of surgery is called "free flap" surgery. The reconnection of your flap will include "microsurgery" (described above) to make sure the blood supply to the "free flap" is healthy.